Getting Started with SleepTite/SleepRite®
SleepTite/SleepRite is a non-pharmaceutical, mechanical, therapeutic treatment that is used to address the root cause of the inflammation in your eyes. The material is both latex free and hypoallergenic. Each SleepTite/SleepRite box contains 30 pair of single use, interchangeable Lid Seals. Studies have shown that by using SleepTite/SleepRite patients can get relief from the discomfort caused by their eyelids not closing properly during sleep. Users have noted that SleepTite/SleepRite is well tolerated and gentle on eyelashes and tissue around the eye.
The proper placement of SleepTite/SleepRite on your eye will be critical to your success with the product. If you are not accustomed to having your eyes occluded at night it is best to start using SleepTite/SleepRite on one eye, until you are comfortable and readily capable of handling its removal and replacement on the eye in the event you have to get up during the evening. Most eye doctors will start the patient off using SleepTite/SleepRite on the eye that bothers them the most and have them do that for at least 30 days. This will give you ample time to work out your nighttime routine and also give you experience with the continued proper removal and replacement of the eye seal during actual nighttime use. If you are a patient used to using other products that occlude both eyes, you should still only start using SleepTite/SleepRite after you have practiced removing and subsequently reapplying at least one of the devices when you need to get up at night.
Overview
- Inadequate Lid Seal (ILS) encompasses many conditions which result in the eyelids not sealing properly at night, including but not limited to, nocturnal lagophthalmos, FES, Bell’s Palsy, lid laxity, and ectropion/entropion
- Most ILS is often present at birth but may develop with age
- Anatomically, the eyelids should slightly overlap and touch (or seal) overnight
- If the seal is not present, the patient has ILS
- The result is Nocturnal Evaporative Stress (NES) resulting in morning symptoms and numerous ocular sequelae
Background
 We often think about our dry eye patients' daytime experiences and how these may exacerbate their symptoms. But in fact, the greater culprit may be lurking in a patient's nighttime environment. Consider that 61% of symptomatic dry eye patients across the spectrum of disease severity have compromised lid closure.
We often think about our dry eye patients' daytime experiences and how these may exacerbate their symptoms. But in fact, the greater culprit may be lurking in a patient's nighttime environment. Consider that 61% of symptomatic dry eye patients across the spectrum of disease severity have compromised lid closure.
If you have a patient whose dry eye is not improving despite treatment, it's time to consider inadequate eyelid closure, sometimes referred to as nocturnal lagophthalmos. This form is far less obvious, as this under-identified and under-treated condition is caused by nocturnal evaporative stress (NES) and is highly prevalent in refractory dry eye.
Exposure secondary to lid lag or lid misalignment perpetuates inflammation that is extremely difficult to manage as are the resultant changes that occur within the lids and ocular surface. Keeping the eye(s) sealed shut at night is a definitive treatment to address the root cause of the inflammation that can occur all night long.
Our eyes don't produce as many tears while we're sleeping, which automatically puts patients in a dry eye state during sleep. Closed lids protect the eye from desiccation. However, many patients' lids don't adequately close at night. Several factors contribute to the development of NES, many of which are directly linked to inadequate lid seal (ILS). These include floppy eyelid syndrome, surgical cosmetic procedures and injections, lid deformities, age-related lid laxity, dermatochalasis, senile ectropion and Graves' disease.
In addition, patients with NES often have another condition, such as meibomian gland dysfunction (MGD), that contribute to the disease. Environmental factors likewise should be considered. A fan in the bedroom, CPAP devices or forced air heat can make symptoms worse. Newer research indicates that even in the majority of patients who show no apparent lid abnormalities, insufficient lid seal is present and leads to nighttime dryness.
Additional Reading: Defeating Dryness
Diagnosis
 The diagnosis is made by asking the patient how their eyes feel upon waking (and during the night). If the answer is anything other than "that's the best they feel" (when they first wake up) then the patient becomes a candidate to trial SleepTite/SleepRite. In the absence of a severe staph blepharitis or demodex infestation, the discomfort felt is most likely due to lid lag or misalignment causing the exposure.
The diagnosis is made by asking the patient how their eyes feel upon waking (and during the night). If the answer is anything other than "that's the best they feel" (when they first wake up) then the patient becomes a candidate to trial SleepTite/SleepRite. In the absence of a severe staph blepharitis or demodex infestation, the discomfort felt is most likely due to lid lag or misalignment causing the exposure.
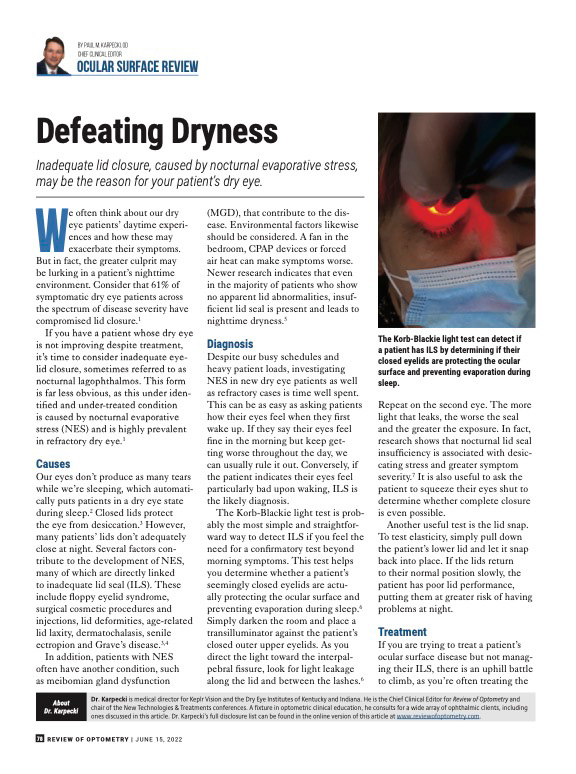
The Korb-Blackie light test is probably the most simple and straightforward way to detect ILS if you feel the need for a confirmatory test beyond morning symptoms. This test helps you determine whether a patient's seemingly closed eyelids are actually protecting the ocular surface and preventing evaporation during sleep.6 Simply darken the room and place a transilluminator against the patient's closed outer upper eyelids. As you direct the light toward the interpalpebral fissure, look for light leakage along the lid and between the lashes.6 Repeat on the second eye.
The more light that leaks, the worse the seal and the greater the exposure. In fact, research shows that nocturnal lid seal insufficiency is associated with desiccating stress and greater symptom severity.7 It is also useful to ask the patient to squeeze their eyes shut to determine whether complete closure is even possible.
Another useful test is the lid snap. To test elasticity, simply pull down the patient's lower lid and let it snap back into place. If the lids return to their normal position slowly, the patient has poor lid performance, putting them at greater risk of having problems at night.
Additional Reading: Dry Eye Disease with Morning Symptoms
Treatment
 If you are trying to treat a patient's ocular surface disease but not managing their ILS, there is an uphill battle to climb, as you're often treating the resulting inflammation, corneal staining or desiccation, MGD and blepharitis without treating the cause. For that reason, a treatment that addresses the lids would be ideal; however, until now, these options were limited.
If you are trying to treat a patient's ocular surface disease but not managing their ILS, there is an uphill battle to climb, as you're often treating the resulting inflammation, corneal staining or desiccation, MGD and blepharitis without treating the cause. For that reason, a treatment that addresses the lids would be ideal; however, until now, these options were limited.
SleepTite/SleepRite is a single-use, hypoallergenic, latex-free device intended to hold the eye closed to prevent NES due to inadequate lid closure. Each card has two eye covers that can be applied universally to either eye. Instructions are straightforward and it's best to begin with having the patient close one eye overnight.

Patients are instructed to place the eye cover over the closed eye. The tab can be oriented laterally or medially for best fit. Gently seal the cover by running a finger around the entire edge of the oval. Upon awakening, the patient easily removes the eye cover by gently grasping the colored tab and pulling in a downward direction so that the eye is not opened during removal. The device should then be discarded. If they find they are not getting up often during the night and the device is working well for them, they can transition to bilateral placement.
Additional Reading: Managing Dry Eye.pdf
Usage Tips
-Dr. Paul Karpecki, O.D., F.A.A.O.
1. Explain to the patient that SleepTite/SleepRite is a non-pharmaceutical, mechanical, therapeutic treatment that will address the root cause of the inflammation and that studies have shown that the treatment can reduce dependency on multiple treatment modalities.
2. Do not sample, simply demonstrate SleepTite/SleepRite on one eye in office and remove.
3. Prescribe a package of 30 sheets (60 SleepTite/SleepRite).
4. Instruct the patient to clean thoroughly around the upper and lower eye lids and dry prior to applying SleepTite/SleepRite.
5. Objectively select the eye that the patient should wear SleepTite/SleepRite or let the patient subjectively select the eye in which they feel most discomfort (at night or in the morning) to monocularly wear SleepTite/SleepRite for the first 4 weeks. This will give the patient the time to properly place and wear the device as well as evaluate the difference between the eye utilizing SleepTite/SleepRite and the eye which remains uncovered while sleeping.
6. If the patient is able to see light or blurry image through SleepTite/SleepRite this indicates that the eye is not completely closed and the device must be reapplied. The reapplication should include more firmly closing the eye and at the same time raising the redundant upper eye lid tissue so that the SleepTite/SleepRite is not adhered to any redundant skin.
7. Typically the patient will place SleepTite/SleepRite on so the tab is located temporally as this is the easiest application to then remove it when awake. If the patient is dislodging SleepTite/SleepRite while sleeping have them place the tab nasally.
8. Instruct the patient NOT to use any gels or ointments prior to using SleepTite/SleepRite. The use of gels or ointments can cause the device to lose adhesion during sleep.
9. Recall the patient in 4 to 6 weeks to reevaluate their ability to use the product successfully. Stress to the patient the importance of continued proper placement and routinely wearing the SleepTite/SleepRite as directed until their follow-up visit.
10. When a patient moves to a bilateral utilization of SleepTite/SleepRite instruct them to remove one or both of the devices if they need to get up at night, and simply place them on the card from which they were removed, and reapply when they return to bed.
Additional Reading: SleepTite/SleepRite Overview
Testimonials

"I love SleepTite/SleepRite for my office and for my patients! When I need a safe, comfortable way to keep my patient's eye(s) sealed overnight I reach for SleepTite/SleepRite. My patients with ILS issues regardless of the cause can't believe the difference SleepTite/SleepRite makes for them."
"Incomplete lid seal (ILS) has become an important characteristic to assess in our dry eye patients. Identifying this anatomical anomaly is critical because it is often the answer to alleviating the signs and symptoms our patients experience. SleepTite/SleepRite provides us a simple solution for these patients and provides a seal that fosters a more normal environment for these patients."


"It's shocking how many patients have morning symptoms as a result of inadequate lid seal (ILS) as a root cause of their dry eye. I've found that SleepTite/SleepRite not only dramatically reduces their symptoms, but it makes all other conventional treatments much more efficacious."
"SleepTite/ SleepRite is my first choice to combat morning dryness from CPAP machines in those with Obstructive Sleep Apnea. STSR does not interfere with the fit of CPAP and protects the ocular surface while the patient sleeps.


"Incomplete lid seal is one of the easiest diagnoses to make and requires no extra equipment. When a patient experiences morning dry eye, this alerts me to look for the presence of ILS. Careful observation of this seemingly small detail can have a profound impact on the outcome of dry eye patients."
"Dry eye is a multifactorial and complex disease that can be challenging to treat. Incomplete lid closure is a common risk factor for dry eye patients, and it must be treated if diagnosed. SleepTite/SleepRite offers a simple and efficacious treatment option to help patients that suffer from incomplete lid seal issues."


"I have found that the number one cause of non-responsive dry eye is inadequate lid seal (ILS). The diagnosis is easy because patients have morning symptoms rather than late in the day symptoms like most dry eye. Thanks to SleepTite/SleepRite we have an extremely effective treatment that has finally relieved patient symptoms and prevents further damage to their meibomian glands."
"My patient's feedback and the improvement in their ocular health has made SleepTite/SleepRite my go to when addressing incomplete lid closure. It is safe, easy and effective."

"I've made the evaluation for incomplete lid seal (ILS) a part of my standard dry eye work up! Asking patients when their symptoms are worse helps me with the diagnosis. Morning symptoms are usually an indicator of ILS. SleepTite/SleepRite has become my go to treatment and has improved the quality of life for many of my OSD patients."
